This guide aims to educate healthcare workers on X-ray safety. By understanding radiation exposure and following best practices, we can minimize risks and maximize diagnostic benefits.
Understanding Radiation Exposure
What is Radiation?
Ionizing radiation used in medical imaging plays a key role in today’s healthcare. During X-ray procedures, this type of radiation goes through body tissues. It creates clear internal images.
These images help doctors diagnose and plan treatments. While this technology is essential, knowing how it works helps us understand why protection is so important.
Different clinical settings present different exposure scenarios. For example, in general radiography, exposure is usually brief and focused. In contrast, fluoroscopy procedures may involve longer exposure times.
Modern imaging systems address these differences with features like pulsed fluoroscopy and digital detectors. These tools greatly reduce radiation doses while still giving high-quality images.
Health Risks of Radiation Exposure
Healthcare workers need to be aware of both the immediate and long-term effects of radiation exposure. The risks of high-dose exposure are well-known. However, we should also pay attention to the effects of low-dose exposure. Possible health impacts include:
Long-term Effects
- Increased risk of cancer, especially in sensitive tissues
- Potential genetic effects
- Cataracts in healthcare workers who are exposed for long periods
Fortunately, new imaging technology has changed how we manage these risks. Digital imaging systems now provide excellent image quality at lower radiation doses. Real-time dose monitoring ensures that exposure stays within safe limits. Smart collimation and beam filtration automatically adjust radiation output for each procedure, offering protection without sacrificing diagnostic quality.
Safety Protocols and Key Principles of Radiation Protection
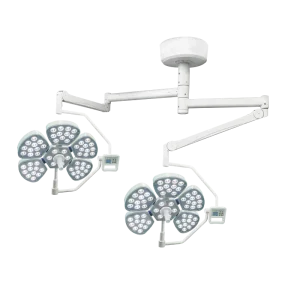
Equipment Maintenance and Safety Features
Regular maintenance and proper operation of X-ray equipment are crucial for radiation safety. Key safety features include:
Beam Limitation Devices:
- Automatic collimation systems that control the radiation field
- Built-in filters to remove unnecessary low-energy radiation
- Digital exposure controls that optimize technical factors automatically
Quality Control Procedures:
- Daily checks to warm up equipment and assess performance
- Weekly image quality evaluations
- Monthly consistency tests on output
Modern X-ray systems incorporate these features into their design, making it easier to follow safety protocols. Digital interfaces provide clear feedback on exposure parameters, helping operators maintain the best settings for each procedure.
Personal Protective Equipment (PPE)
Using PPE correctly is vital for protecting against radiation. Essential protective gear includes:
Lead Aprons:
- Designed for comfort during long procedures
- Different lead equivalencies for various exposure scenarios
- Regular testing to check for damage using specialized imaging tools
Additional Protection:
- Thyroid shields for upper body procedures
- Lead glasses with side protection for eye safety
- Mobile shields for extra protection during complex procedures
“The right PPE can make all the difference during long procedures,” says Jane Doe, a Radiology Technician
Effective Use of Protective Equipment
Wearing protective gear like lead aprons is one of the best ways to reduce radiation risk. Regular checks for wear or damage are essential since compromised equipment can lead to increased exposure. Additionally, using thyroid collars and other accessories gives extra layers of protection during imaging.
Justification
Before any X-ray procedure begins, it’s important to ask, “Is this necessary for the patient’s care?” This principle emphasizes weighing benefits against potential risks. Just like checking the weather before planning an outing, healthcare professionals must evaluate whether the advantages of an X-ray outweigh any associated hazards.
Optimization (ALARA Principle)
The ALARA principle—”As Low As Reasonably Achievable”—is our goal in radiation safety. It means we strive to minimize radiation exposure while still getting necessary diagnostic outcomes. Practically speaking, this involves:
- Choosing appropriate settings tailored to each patient.
- Using advanced features like automatic exposure control.
- Making sure patients are positioned correctly on the first attempt to avoid unnecessary retakes.
Dose Limitation
Keeping track of radiation exposure has become easier with new digital tools. Clear limits are set for both patients and healthcare staff to ensure safety is maintained. Real-time monitoring systems provide instant feedback on exposure levels, allowing quick adjustments when needed.
Limiting Exposure Time
Managing how long someone is exposed to X-rays is crucial in reducing overall doses. Each imaging procedure should be planned carefully so that X-rays are used only as long as necessary to gather essential diagnostic information.
Regular Equipment Maintenance and Calibration
Consistent maintenance and calibration of X-ray equipment are vital for ensuring safety and efficiency. Well-maintained machines produce better images and help minimize unnecessary radiation exposure.
Training and Education
Getting Started Right
Remember your first day working with X-ray equipment? Everyone starts somewhere! Good training builds confidence and keeps everyone safe. Here’s what works:
- Hands-on practice with equipment features.
- Clear explanations of safety protocols.
- Regular check-ins with experienced staff.
Modern systems include training modes and guided workflows that help new staff learn safely.
Keeping Skills Sharp
Healthcare keeps changing, so our skills should too! Ongoing education isn’t just about ticking boxes—it’s about staying sharp and safe. Regular updates help you:
- Learn new techniques that reduce exposure.
- Understand equipment updates.
- Stay current with safety guidelines.
Many facilities now use digital training tools that make learning convenient and practical. Quick refresher sessions fit easily into busy schedules.
Setting Up a Safety Program
Building Your Program
Creating a safety program is like building a house—you need a solid foundation. Start with:
Basic Components:
- Clear safety policies everyone understands.
- Well-defined roles for team members.
- Regular schedules for safety checks.
- Easy-to-follow emergency procedures.
Modern equipment makes this easier with built-in safety features and clear user interfaces.
Keeping Track
Monitoring radiation exposure shouldn’t be stressful. Today’s digital tools make it simple:
- Personal radiation badges that track exposure automatically.
- Area monitors that alert you to any issues.
- Easy-to-read reports showing trends over time.
The best part? Modern systems can collect and organize this data automatically, saving time while improving safety.
Bringing It All Together
Safety in X-ray departments depends on three key things: good equipment, well-trained staff, and clear rules. When these come together, everyone benefits:
- Patients get safe, clear images, helping doctors make accurate diagnoses without unnecessary risks.
- Staff feel secure and confident, knowing they’re using the right tools and following the best safety steps.
- Facilities meet their goals easily, earning trust and staying compliant with safety standards.
By focusing on safety and always looking for ways to improve, X-ray teams can create a better experience for everyone.
Let’s work together to raise the bar in X-ray safety—contact us today to see how we can help your team thrive.