Radiology report structures are far from one-size-fits-all. Their design often reflects the unique workflows, clinical priorities, and institutional preferences of healthcare facilities. This diversity ensures radiologists can tailor reports to best serve their intended audience, but it can also lead to inconsistencies that challenge standardization and interpretation. Below, we delve into the most common variations, enriched with examples and additional insights to bring these concepts to life.
1. Standardization vs. Customization
Standardized guidelines such as those from the American College of Radiology (ACR) or European Society of Radiology (ESR) provide a framework to ensure consistency in radiology reports. However, many institutions customize their reports to reflect specific clinical focuses, patient demographics, and internal protocols.
- Standardized Guidelines: A standard chest X-ray report might simply follow a template stating the technique, findings, and impression, ensuring uniformity across different radiologists.
- Customized Reports: On the other hand, a specialized oncology center may modify its reports to include advanced metrics like RECIST (Response Evaluation Criteria in Solid Tumors) to monitor treatment efficacy. Such additions allow for more actionable insights for oncologists.
Example:
A general abdominal CT report might state, “No acute abnormalities noted.”
In contrast, a report from a liver transplant center might add, “No evidence of portal vein thrombosis; hepatic parenchyma appears homogeneous without significant fibrosis.” This additional specificity supports the transplant team in making informed decisions.
2. Section Inclusion
Different institutions often add or omit sections based on the imaging studies performed or the specialties served. These additions help cater to the unique needs of specific patient populations or clinical scenarios.
- Specialty Additions: A breast imaging report might include sections for BI-RADS (Breast Imaging-Reporting and Data System) categories to standardize breast cancer risk assessment, while a musculoskeletal imaging report may describe joint alignment or muscle injury gradings in greater detail.
- Unique Protocols: Pediatric-focused institutions may incorporate sections addressing congenital anomalies, while trauma centers might highlight injury severity scores.
Example:
A pediatric abdominal ultrasound report might include, “No evidence of intussusception or appendicitis,” emphasizing conditions common in children. Conversely, an adult-focused institution may prioritize findings like hepatic steatosis or cholelithiasis.
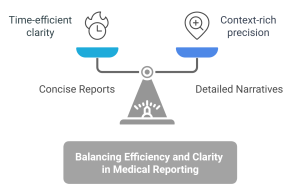
3. Detail Level
The level of detail in radiology reports can range from concise summaries to elaborate narratives. These differences often stem from the radiologist’s experience, the imaging modality used, and the intended audience.
- Concise Reports: Designed for efficiency, these reports focus on key findings. For instance, a chest X-ray for pre-operative clearance might read, “No acute cardiopulmonary abnormalities.”
- Detailed Narratives: In contrast, a radiologist specializing in interstitial lung disease might provide an in-depth analysis, stating, “Diffuse reticular opacities predominantly in the lower lobes, with traction bronchiectasis, consistent with fibrotic hypersensitivity pneumonitis.”
Pros and Cons:
Concise reports save time but might omit valuable context, while detailed reports provide clarity at the expense of brevity. Striking the right balance is crucial for effective communication.
4. Impression and Recommendations
The impression section summarizes critical findings and often includes recommendations. Variations here can significantly influence patient management.
- Clarity and Actionability: A clear impression might state, “Findings consistent with acute appendicitis. Recommend surgical consultation.”
- Ambiguous Reports: Conversely, a vague impression like, “Mild thickening of the appendix; clinical correlation suggested,” could lead to delays in decision-making.
Enhancing Recommendations:
Incorporating clinical context can make recommendations more actionable. For example, a radiologist aware of a patient’s history of recurrent urinary tract infections might recommend follow-up imaging for kidney stones, even if findings are subtle.
5. Use of Templates
Structured templates enhance consistency, reduce errors, and ensure all critical elements are addressed. However, these templates may vary widely across modalities and specialties.
- Consistency Through Templates: A mammogram report template might include:
- Patient demographics
- Study indication
- Findings categorized by quadrants
- BI-RADS score
- Recommendations
- Specialized Formats: A cardiac MRI report might emphasize parameters like left ventricular ejection fraction (LVEF), myocardial perfusion, and late gadolinium enhancement patterns. Check out this guide to radiology report templates for more details.
Example:
A breast imaging report using BI-RADS might state, “Category 3: Probably benign. Recommend follow-up mammogram in six months.”
In comparison, a general X-ray report might simply note, “No acute findings.”
6. Follow-Up Recommendations
Follow-up imaging recommendations vary among institutions and radiologists, reflecting differences in training, experience, and patient populations.
- Influencing Factors: Recommendations for lung nodules, for example, might differ:
- Experienced Radiologist: “A 6-month follow-up CT is recommended to monitor the stable nodule.”
- Less Experienced Radiologist: “Clinical correlation and consideration for follow-up imaging suggested.”
Example:
For a patient with a detected lung nodule:
- Institution A might recommend, “Routine follow-up CT in 12 months.”
- Institution B might suggest, “Consider PET/CT to assess metabolic activity.”
7. Technical Details
The technical section of a report often varies in depth, depending on institutional preferences and the complexity of the study.
- Basic Reports: A community hospital might note, “CT scan performed with contrast.”
- Advanced Reports: Academic centers may provide detailed descriptions, such as, “CT chest performed with intravenous iodinated contrast (100 mL Iohexol 350) at a flow rate of 4 mL/sec; acquisition in the arterial phase.”
Example:
For a brain MRI:
- Basic report: “MRI performed with and without contrast.”
- Advanced report: “3T MRI brain with and without gadolinium contrast, axial T2-weighted, FLAIR, DWI, and ADC sequences acquired.”
8. Clinical Contextualization
Incorporating clinical context into reports ensures that findings are relevant and actionable for referring physicians.
- Detailed Context: A report might read, “Findings of right lower lobe consolidation with pleural effusion, consistent with pneumonia in the clinical context of fever and productive cough.”
- Minimal Context: In contrast, a less informative report might state, “Right lower lobe consolidation noted.”
Example:
For an abdominal ultrasound:
- Minimal Context: “Gallbladder sludge noted.”
- Contextualized: “Gallbladder sludge noted; patient history of biliary colic suggests early cholecystitis.”
Why These Variations Matter
Understanding these variations is critical for healthcare professionals interpreting radiology reports. Recognizing the nuances in structure, detail, and recommendations can improve communication, enhance clinical decision-making, and ultimately lead to better patient outcomes. Patients, too, benefit from greater transparency and clarity when reports are tailored to their specific clinical contexts.
Wrap-up
Radiology report structures are as diverse as the institutions that produce them. While variability can pose challenges, it also reflects a commitment to personalized care and specialization. Emphasizing clarity, clinical relevance, and standardization where possible ensures that radiology reports remain indispensable tools in modern medicine. Navigating these complexities with an understanding of institutional preferences and patient needs is a key skill for radiologists and referring physicians alike.